Dr. João Sérgio Neves is an endocrinologist, based in the Faculty of Medicine of the University of Porto and São João Hospital in Porto, Portugal. Dr. Neves’s team submitted a research proposal to access Vivli to conduct analysis relevant to their topic, “Albiglutide and Cardiovascular Outcomes in Type 2 Diabetes With and Without Concomitant Sodium-Glucose Cotransporter-2 Inhibition Use”. The team’s completed research has been presented in publications including the Journal of the American College of Cardiology. Dr. Neves sat down with Vivli to tell us more about accessing individual participant data to advance his research, and the potential for combination therapy to reduce the risk of cardiovascular events in patients with Type 2 Diabetes.
Dr. João Sérgio Neves is an endocrinologist, based in the Faculty of Medicine of the University of Porto and São João Hospital in Porto, Portugal. Dr. Neves’s team submitted a research proposal to access Vivli to conduct analysis relevant to their topic, “Albiglutide and Cardiovascular Outcomes in Type 2 Diabetes With and Without Concomitant Sodium-Glucose Cotransporter-2 Inhibition Use”. The team’s completed research has been presented in publications including the Journal of the American College of Cardiology. Dr. Neves sat down with Vivli to tell us more about accessing individual participant data to advance his research, and the potential for combination therapy to reduce the risk of cardiovascular events in patients with Type 2 Diabetes.
Could you tell us a little bit about your research? What got you interested in the particular area of research that you carried out working with Vivli?
So I am a clinical endocrinologist; I do clinical research in the field of Endocrinology. I have a particular interest in the effects of endocrine diseases on cardiovascular risk and on cardiac function. My main areas of research have been obesity, diabetes, and pre-diabetes. Previous studies conducted by our team have explored the effects of GLP-1 receptor agonists in patients with diabetes, both with and without heart failure. One of the questions that was still unanswered from the literature was whether the benefits of GLP-1 receptor agonists were still observed in those that were already treated with SGLT2 inhibitors. These two classes of drugs are known to be protective from a cardiovascular perspective for patients with Type 2 Diabetes. However, the two classes were developed and the clinical trials were conducted in parallel. So when clinical trials of GLP-1 receptor agonists (AMPLITUDE-O trial and Harmony Outcomes study) were conducted a bit later and included participants that were already treated with SGLT2 inhibitors at baseline. The authors of the AMPLITUDE-O trial had already performed a sub-analysis evaluating the effects of the GLP-1 receptor agonists in patients treated with SGLT2 inhibitors. Given the relevance of further exploring the combination of GLP-1 receptor agonists with SGLT2 inhibitors, our group requested the Harmony Outcomes study from Vivli. The we also performed a meta-analysis combining the results of the Harmony Outcomes study with the results from the AMPLITUDE-O trial. So there are two trials that we included that evaluate the effects of GLP-1 receptor agonists and included some patients using SGLT2 inhibitors and we wanted to know if this data could help us understand if both drugs when combined can give further cardiovascular protection to patients with Type 2 Diabetes.
And having come to the conclusions that you did – that there may be further reduction in cardiovascular risk but that more clinical trials with combination therapy are required – have the findings from this made any impact in terms of research practice that you’re aware of, since the findings have become available?
So since the findings became available, there has been some interest from other doctors contacting us on how to interpret our findings. We are very cautious and we believe that further data and dedicated clinical trials are necessary to thoroughly evaluate this drug combination. However, acknowledging that these trials might take several years to be conducted, we also recognize that our existing data could assist physicians in making informed decisions about utilizing this combination in the interim. We believe that the results of the Harmony Outcomes trial, in combination with the AMPLITUDE-O trial, favor the possibility that the combination of both drugs is protective from a cardiovascular perspective.
Interestingly, in the same month our paper was published in the Journal of the American College of Cardiology, the European Society of Cardiology published an updated guideline on the treatment of patients with Type 2 Diabetes and cardiovascular disease, and they recommended that patients with Type 2 Diabetes and cardiovascular disease should be treated with both drugs. They did not yet cite our paper because it was published just before publication of the guideline, but they do cite, for example, the AMPLITUDE-O trial. So I believe that our data will reinforce this recommendation; and we see that the field of treatment and prevention of cardiovascular disease in Type 2 Diabetes was already moving in the direction of our findings. But as there was only one study evaluating this combination, we think that our results will be very important for supporting the use of GLP-1 receptor agonists in combination with SGLT2 inhibitors.
Can you talk a little bit about using the data that was available through Vivli; what were you able to do using that data that you were not able to do otherwise?
The type of analysis we aimed to conduct could theoretically be performed using observational data. However, utilizing observational data poses significant challenges due to numerous confounders, particularly when assessing the effects of therapeutic interventions involving drugs. This limitation is well-documented, and such an approach would lack robustness, potentially raising more questions than providing answers. I think that the most interesting thing about the analysis that we performed was that this was a clinical trial that was already performed; the data was already available.
When we analyzed the data we worked with the authors from the primary paper; we got in contact with the authors of the primary analysis and we planned this analysis together. Our interactions with the original authors were invaluable in interpreting the data, given their familiarity with it. This collaborative effort resulted in an interesting analysis and yielded important results.
Can you talk a little bit about your experience of working with the Vivli platform – the processes and technology and what that was like?
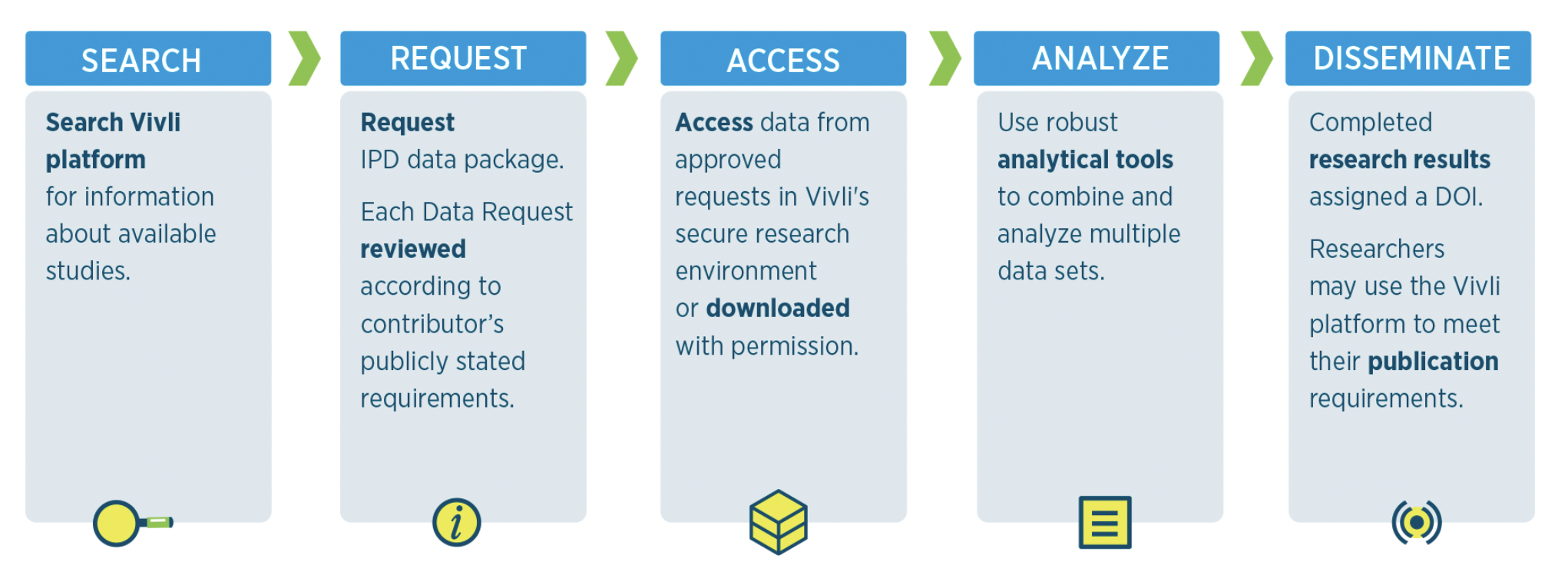
I think that the process was quite easy, the instructions are clear. We know that there is always some type of bureaucracy that is involved, but that’s part of how it works, because we are dealing with data from patients. Of course it is anonymized data but I think that’s not different from what I was used to with other types of shared data. , The process works quite smoothly.
The thing that I feel that was a little bit different from our previous experience with secondary analyses, was the use of a platform for analyzing the data outside of our computers. Nevertheless, we successfully conducted our data analysis, and the data was also accessible within the remote computer, allowing us to execute the entire analysis seamlessly.
And how did you find out about Vivli and the opportunity to reuse shared data in general?
We had previously conducted analyses through the secondary analysis of existing data, utilizing platforms such as BioLINCC , which incorporates data from studies sponsored by NIH. Our awareness of Vivli stemmed from mentions in papers that disclosed their data sharing approaches, indicating that access could be facilitated through Vivli. This was my first personal experience using Vivli, and I must say that I find the work undertaken by the Vivli team truly remarkable. Your efforts contribute significantly to the future of research and the enhanced utilization of already collected data.
How has the direction of your own research been affected by the research that you did on this project? Has it affected what you’re doing or changed your direction in any way?
I believe it has provided clarity on the next steps to enhance knowledge in this field. In our team, we recognized that addressing whether the treatments were additive or not would be a pivotal question. If we discovered that the combination did not yield additional risk reduction, we needed to understand which drug to select for specific patients. With the results we obtained, our focus shifted towards understanding how to improve access to these drugs and assessing their effectiveness in other populations, particularly in the earlier phases of Type 2 Diabetes and even pre-diabetes. As we design new clinical trials, we are already incorporating the insights gained from this analysis.
Would you use the Vivli platform again? Are there any changes or improvements that you would recommend to how it works?
Certainly, the experience was highly positive, and I look forward to working again with Vivli in the future. One overarching improvement (that’s not specific to Vivli) would be to expand access to even more data. I do believe that the data is very valuable and that it is very important to share the data from large clinical trials. The type of study that we analyzed is probably the most relevant that should be shared – of course with a very specific and detailed analysis plan and with all the regulations that are needed in this context. Considering the substantial resources and time invested in these clinical trials, there is often a wealth of data that remains untapped. Many crucial analyses may not have been conducted and researchers not primarily involved in the clinical trial may be able to identify these questions and answer them using the data from that trial. Therefore, it is important to facilitate access to this valuable resource.
So my main recommendation is to try to increase even further the number of studies that are available. Of course this also depends on the companies that own the data and the drugs that are being evaluated. But our analysis could not be performed without the sharing by GSK, so we are also thankful for their contribution to Vivli and for the sharing of the data.
And is there any advice you would give to other researchers who are at the beginning of the process of requesting or using shared data?
My main advice is to have a very specific question that the researchers want to answer; develop a detailed analysis plan; and submit the request to the Vivli platform. While the process may take some time, it is not overly complex. With patience and adherence to the required steps, one can successfully obtain access to the data. I firmly believe that enhancing the utilization of the Vivli platform and increasing access to data from large clinical trials will significantly improve the quality of knowledge across various fields in medicine.
 Rheumatoid arthritis (RA) poses a significant challenge due to its chronic nature and impact on joint health. While treatments have evolved, achieving remission remains elusive for many patients. Using a dataset from the Vivli repository, Dr. Ricardo Ferreira and a team of researchers delved into examining the assessment criteria for remission in RA, shedding light on the limitations of current approaches and proposing a new model—the dual target strategy.
Rheumatoid arthritis (RA) poses a significant challenge due to its chronic nature and impact on joint health. While treatments have evolved, achieving remission remains elusive for many patients. Using a dataset from the Vivli repository, Dr. Ricardo Ferreira and a team of researchers delved into examining the assessment criteria for remission in RA, shedding light on the limitations of current approaches and proposing a new model—the dual target strategy.

 In a recent study led by Dr. Sarah Nevitt, a senior research associate at the University of Liverpool, a team of researchers examined the effectiveness of various antiepileptic drugs (AEDs) used as monotherapy for people experiencing seizures due to epilepsy. Epilepsy, a common neurological disorder, results from abnormal electrical discharges in the brain, causing recurrent seizures. Typically, around 60% to 70% of individuals with epilepsy achieve longer-term remission, often shortly after beginning treatment with antiepileptic drugs.
In a recent study led by Dr. Sarah Nevitt, a senior research associate at the University of Liverpool, a team of researchers examined the effectiveness of various antiepileptic drugs (AEDs) used as monotherapy for people experiencing seizures due to epilepsy. Epilepsy, a common neurological disorder, results from abnormal electrical discharges in the brain, causing recurrent seizures. Typically, around 60% to 70% of individuals with epilepsy achieve longer-term remission, often shortly after beginning treatment with antiepileptic drugs. Dr. João Sérgio Neves is an endocrinologist, based in the Faculty of Medicine of the University of Porto and São João Hospital in Porto, Portugal. Dr. Neves’s team submitted a research proposal to access Vivli to conduct analysis relevant to their topic, “Albiglutide and Cardiovascular Outcomes in Type 2 Diabetes With and Without Concomitant Sodium-Glucose Cotransporter-2 Inhibition Use”. The team’s completed research has been presented in publications including the
Dr. João Sérgio Neves is an endocrinologist, based in the Faculty of Medicine of the University of Porto and São João Hospital in Porto, Portugal. Dr. Neves’s team submitted a research proposal to access Vivli to conduct analysis relevant to their topic, “Albiglutide and Cardiovascular Outcomes in Type 2 Diabetes With and Without Concomitant Sodium-Glucose Cotransporter-2 Inhibition Use”. The team’s completed research has been presented in publications including the  Did you know there’s more on Vivli than just clinical trial data? The majority of our repository of data comes from clinical trial data, but also includes significant numbers of platform trials, observational studies, and real-world evidence resources.
Did you know there’s more on Vivli than just clinical trial data? The majority of our repository of data comes from clinical trial data, but also includes significant numbers of platform trials, observational studies, and real-world evidence resources.